MD, Tohoku University, Sendai, Japan, 1986, and PhD, Karolinska Institutet, 1998.
The current position is a senior scientist at Karolinska Institutet, CLINTEC, Transplantation Surgery, Stockholm, Sweden.
I trained as a surgeon at a city hospital and also at the Department of Thoracic Surgery in Japan. The specific interest is transplantation immunology. My research topics are immune responses in pig-to-human xenotransplantation, pancreatic islet transplantation, and tolerance induction in organ transplantation. I am currently involved in a clinical project to induce organ-specific tolerance by cell therapy in deceased donor liver transplantation.
Ex-vivo-generated immunomodulatory cells reduce proinflammatory macrophage (M1) polarization
Nils Agren1,2, Kaoru Okada1,2, Rima Alhatour1,2, Daniel mmm Martinez1,2, Awan Ajeenah1,2, Monir Qasha1,2, Ming Yao1,2, Bo-Goran Ericzon1,2, Makiko Kumagai-Braesch1,2.
1Transplantation Surgery, CLINTEC, Karolinska Institutet, Stockholm, Sweden; 2ME Transplantation, Karolinska University Hospital, Huddinge, Sweden
Background: In clinical liver transplantation, the adoptive transfer of donor-specific immunomodulatory cells (DSIMC) has been shown to result in the early withdrawal of general immunosuppression. DSIMC are generated ex vivo by culturing recipients' peripheral mononuclear cells (PBMC) and irradiated donor PBMC with co-stimulation blockers, such as anti-CD80/86 antibodies or CTLA4Ig (belatacept). Macrophages may play a crucial role in maintaining tolerance.
Aim: Here, we investigate whether DSIMC can exert an anti-inflammatory effect to reduce M1 macrophage polarization in vitro in a donor-specific manner.
Methods: PBMC from healthy volunteers were used to generate DSIMC and differentiate macrophages. DSIMC or donor-specific activated cells (DSAC) were generated by co-culturing responder PBMC and irradiated stimulator PBMCs with or without belatacept, respectively. On day 7, the culture medium was changed, and irradiated stimulator cells were replenished. The cultured cells and supernatant were harvested on day 10. For macrophage differentiation, CD14+ cells were cultured with a macrophage medium. On day 10, M1 polarization was performed with LPS and IFN-γ, and different amounts of DSIMC or DSAC were added and incubated for 1 day. Cytokine profiles and macrophage polarization markers were examined
Results: The relative gene expressions of CD25, TGF-beta, and FGL2 were higher in T cells from DSIMC than in those from DSAC. IFN-gamma and IL-10 concentrations in day 10-culture supernatant were lower in DSIMC than in DSAC.
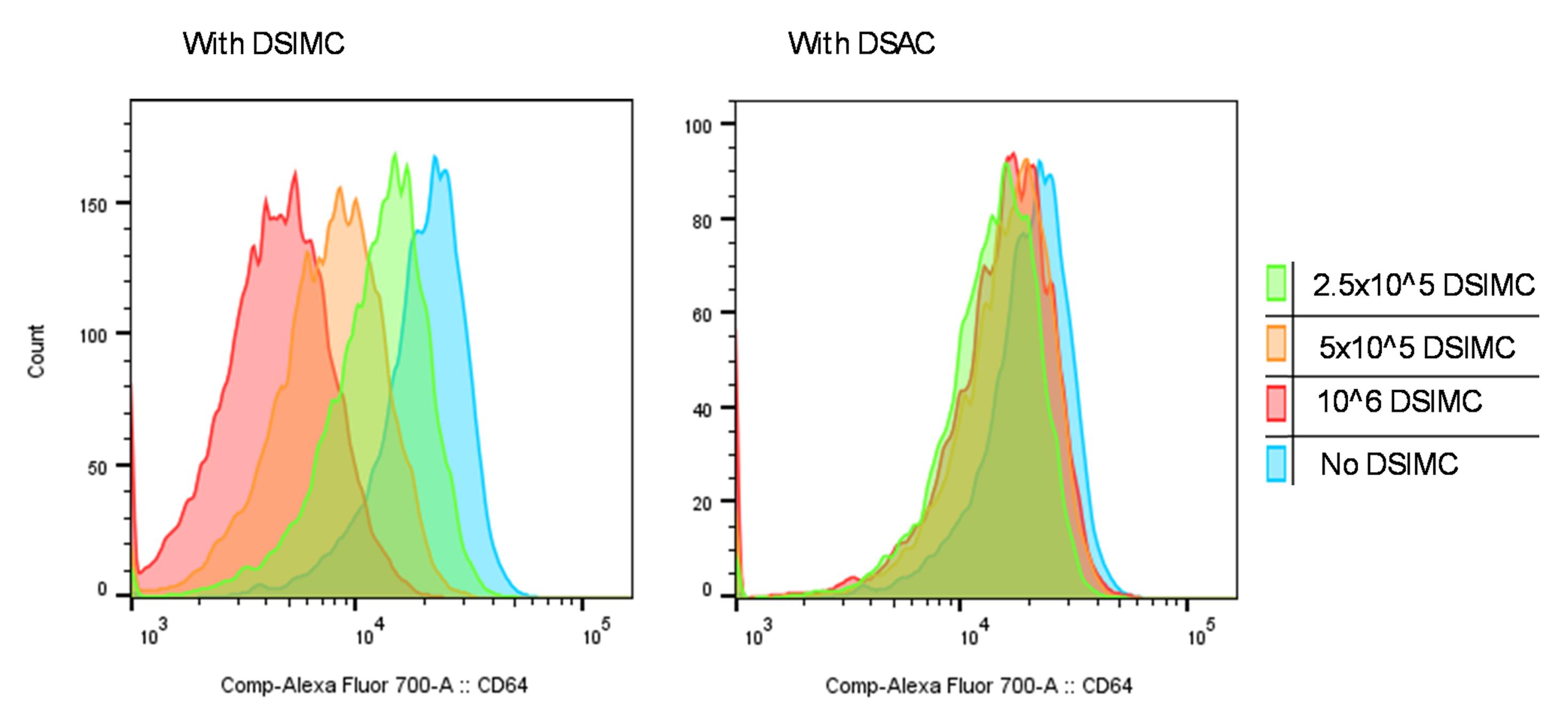
DSIMC, unlike DSAC, suppressed the expression of M1 macrophage markers such as CD64 and CD80 in a dose-dependent manner. This effect was not donor-specific. A typical example of CD64 expression on M1 macrophages after co-culturing with DSIMC and DSAC is shown in Figure 1. Co-culture with DSIMC reduces on M1 macrophage development in a dose-dependent manner, while no significant differences was observed in the group co-cultured with DSAC.
Conclusion: The relative gene expression study indicated that T cells from DSIMC have the potential to produce immunosuppressive cytokines compared to those from DSAC. The DSIMCs have a donor non-specific anti-M1 polarization capacity
These immunomodulatory and anti-inflammatory functions could be important in maintaining the tolerance of transplanted liver grafts.
Vetenskapsrådet, Grant Number: 2018-00845 . Center for Innovative Medicine Grant Number: 2023-2025, 2024-2026, 2025-2027 . Stockholms Läns Landsting Grant Number: 20180606 .
[1] immunomodulatory cells
[2] anti-inflammation
[3] macrophages