
PhD student
Exosomal miR-34a-3p from tubular epithelial cells elicits M1 macrophage polarization in cisplatin-induced acute kidney injury mice
Jingchao Yang1, Longhui Yuan1, Shuyun Liu1, Yanrong Lu1, Yujia Yuan1.
1West China Hospital, Sichuan University, Chengdu, People's Republic of China
Introduction: Acute kidney injury (AKI), characterized by a sudden renal function decline, is a common clinical syndrome. In recent years, it has emerged that, apart from oxidative stress, mitochondrial dysfunction and apoptosis, the renal inflammatory response has been proven to trigger the progression of AKI. Tubular epithelial cells (TECs) represent the central cell type affected by AKI, and are vulnerable to various types of injury (hypoxic, ischemic, toxins, metabolic disorders and senescence). Accumulating evidence shows that injured TECs are key determinant cells in tubulointerstitial inflammation in AKI. Macrophages are primarily cell types involved in promoting renal tubulointerstitial inflammation. Research has suggested that the role of macrophages in the development of AKI is dependent mainly on their phenotype. Proinflammatory M1 macrophages can release inflammatory factors to trigger kidney damage after infection. Recent studies have shown that TECs can communicate with macrophages via extracellular vesicle-dependent information. Therefore, in this study, we explored the role of exosomal miRNA derived from TECs in the development of tubulointerstitial inflammation.
Methods: Firstly, exosomes were isolated from TECs incubated with cisplatin (EXOcisp) or without cisplatin (EXOcon) via differential ultracentrifugation. Then, immunofluorescence, flow cytometry analysis, and molecular approaches were utilized to evaluate the cellular internalization of the exosomes by the macrophages. Mechanistically, we performed this study using a miRNA microarray to identify the differentially abundant miRNAs between EXOcon and EXOcisp.
Results: We demonstrated that EXOcisp could regulate macrophage polarization and the expression of proinflammatory cytokines compared with EXOcon. Global miRNA expression profiling of EXOcon and EXOcisp revealed that miR-34a-3p, which regulated inflammation in obese, rheumatoid arthritis, and cardiac injury models, was significantly elevated in EXOcisp.
Conclusion: We demonstrated that TEC-derived exosomes transfer miR-34a-3p to macrophages, which promotes M1 macrophage polarization. These findings revealed a novel function of exosomal miR-34a-3p as a regulator of macrophage activation and tubulointerstitial inflammation in AKI. The exosome-mediated inflammatory pathway may be a new mechanism responsible for the development of renal inflammation by promoting TEC-macrophage communication.
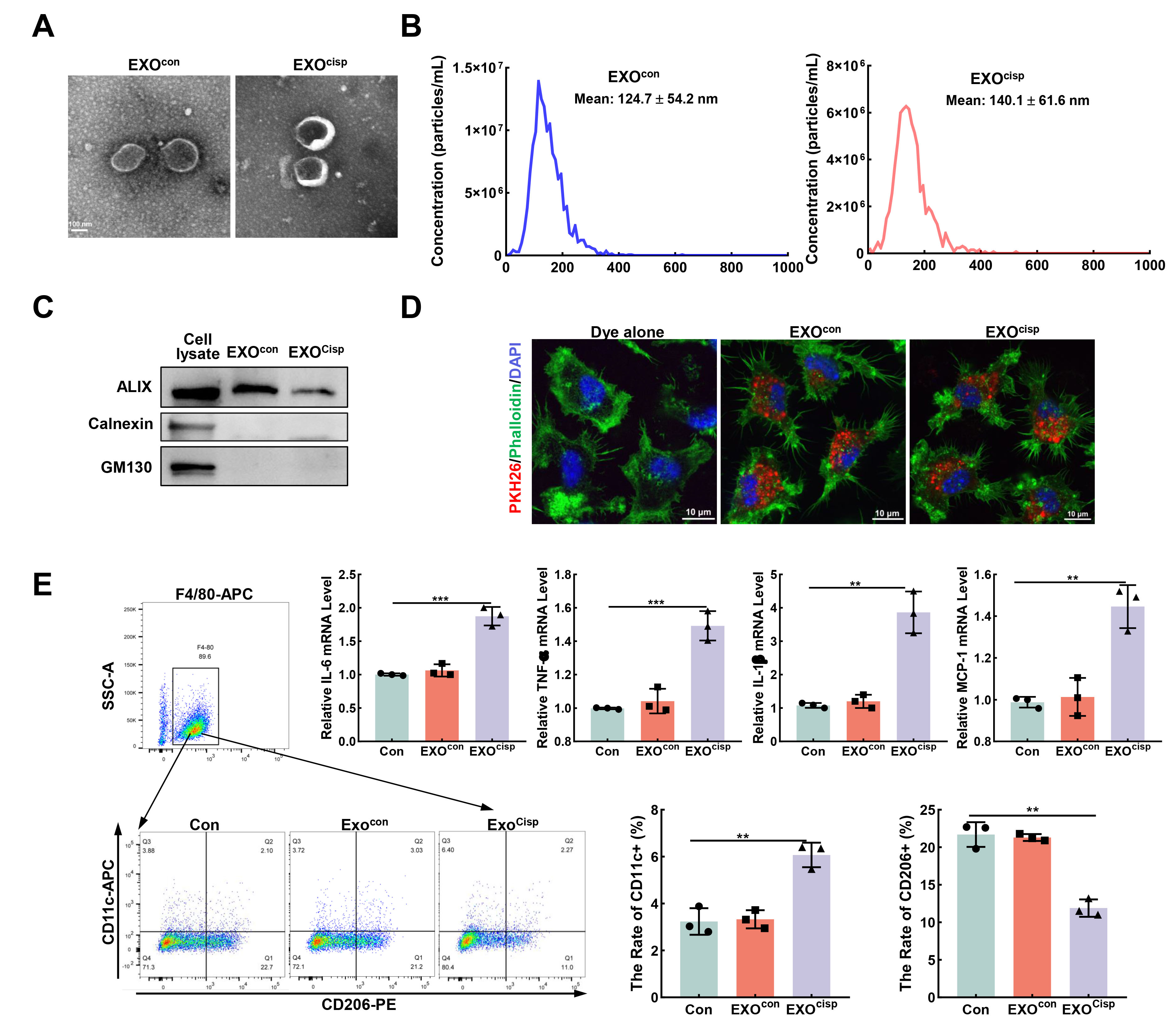
Figure 1. Exosomes derived from cisplatin-treated TECs promote M1 macrophage polarization
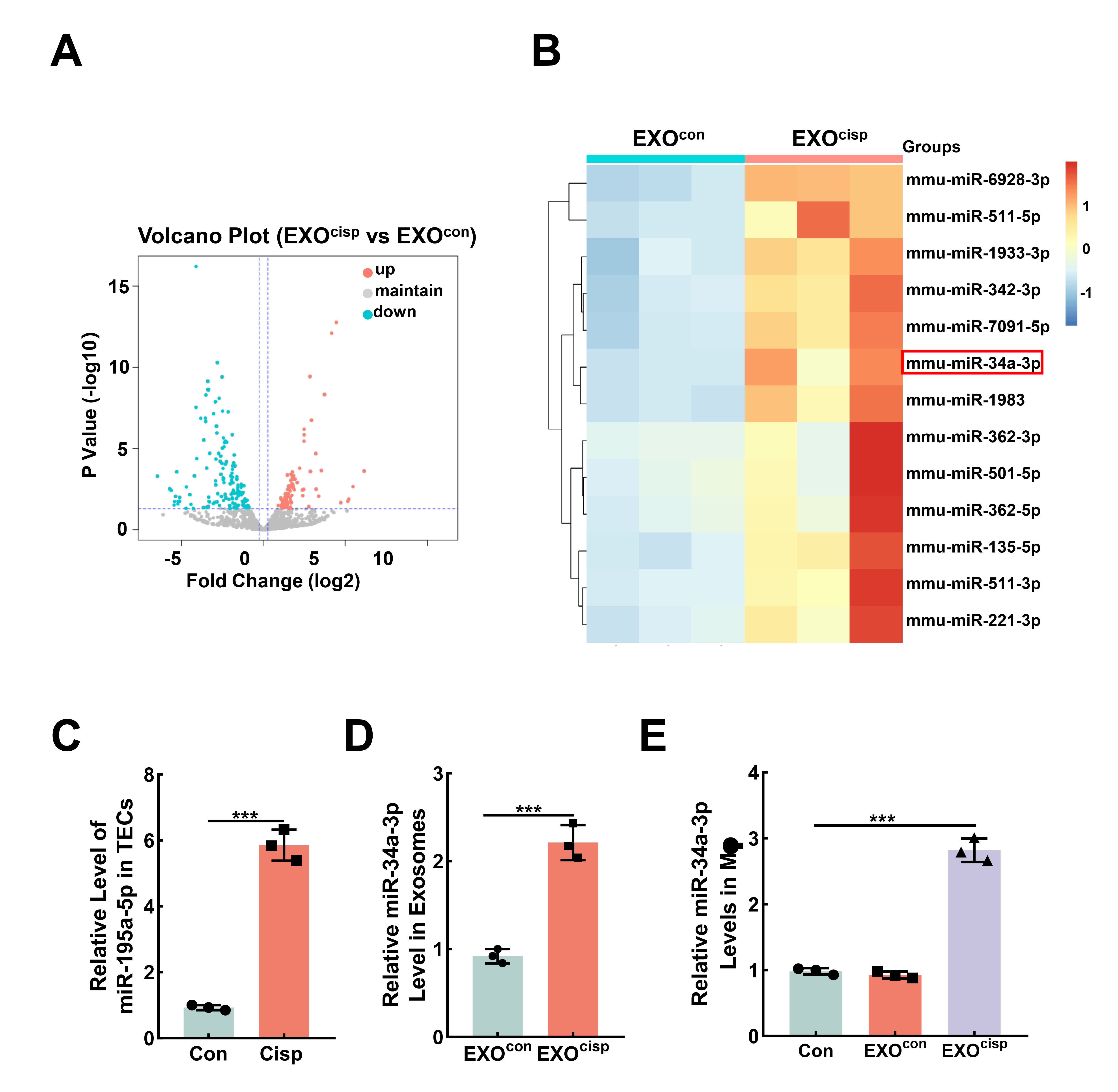
Figure 2. EXOcisp promotes M1 macrophage activation via miR-34a-3p