Cryopreservation of hepatocytes: Impact of long-term storage and organ donor factors on cell quality for clinical applications
Kadriye Güven1, Valeria Iansante1, Sharon Lehec1, Ragai Mitry1, Anil Dhawan1, Celine Filippi1.
1Institute of Liver Studies, King’s College London, King’s College Hospital NHS Foundation Trust, London, United Kingdom
King’s College London Hepatocyte & Cell Therapy Research Group.
 Background: Liver transplantation is the only curative option for end-stage liver disease, but its applicability is limited by donor shortages. Hepatocyte transplantation offers a promising alternative, particularly for paediatric acute liver failure, yet its success relies on the availability of viable cells. Cryopreservation enables off-the-shelf use, but long-term storage may impair cell quality. This study investigates how cryostorage duration, donor characteristics, and organ retrieval parameters affect the viability and functionality of cryopreserved primary human hepatocytes (PHHs).
Background: Liver transplantation is the only curative option for end-stage liver disease, but its applicability is limited by donor shortages. Hepatocyte transplantation offers a promising alternative, particularly for paediatric acute liver failure, yet its success relies on the availability of viable cells. Cryopreservation enables off-the-shelf use, but long-term storage may impair cell quality. This study investigates how cryostorage duration, donor characteristics, and organ retrieval parameters affect the viability and functionality of cryopreserved primary human hepatocytes (PHHs).
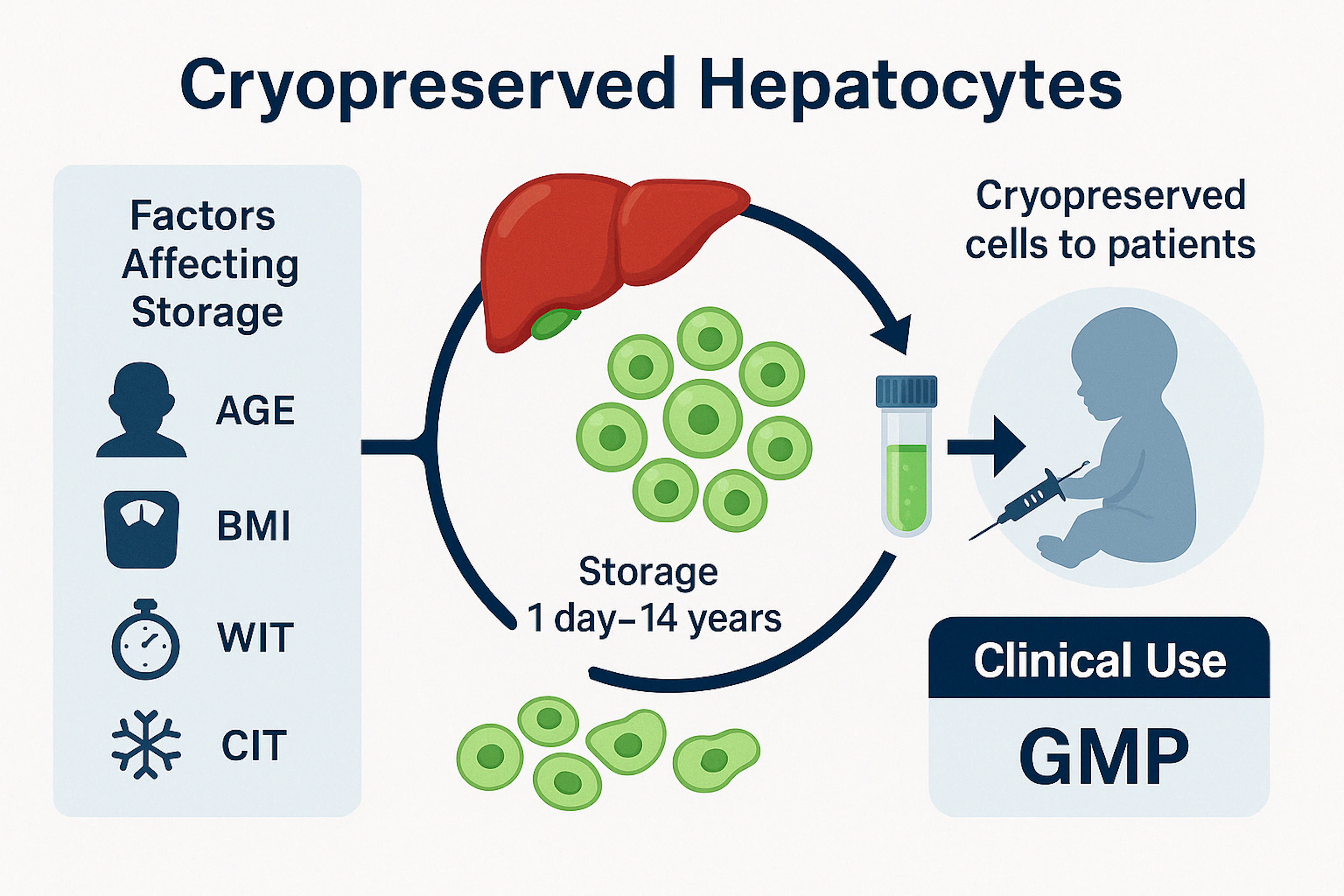
Methodology: To investigate how the duration of cryostorage influences the post-thaw viability and functionality of PHHs, and to assess the impact of donor-related factors, including age, body mass index (BMI), warm ischemia time (WIT), and cold ischemia time (CIT), on overall cell quality. We conducted a retrospective analysis of 144 thawing events across 81 GMP-grade hepatocyte batches cryopreserved for up to 14 years. Donor age ranged from 3 days to 70 years. Viability and functionality were assessed using MTT assays, albumin and urea secretion, and CYP450 activity. Linear regression was used to assess correlations (p < 0.05 considered significant).
Results: Cryopreservation duration had no significant impact on hepatocyte viability or function, confirming that clinical-grade PHHs can maintain quality for up to 14 years. In contrast, donor age correlated negatively with post-thaw viability (R² = 0.035, p = 0.029), yield (R² = 0.039, p = 0.041), and metabolic activity (R² = 0.278, p = 0.008), while showing a positive correlation with induced EROD function (R² = 0.432, p = 0.020). Donor BMI showed significant negative associations with viability (R² = 0.075, p = 0.003), yield (R² = 0.069, p = 0.011), and metabolic activity (R² = 0.267, p = 0.019). CIT showed a weak negative correlation with viability (R² = 0.151, p < 0.0001), particularly below 60% viability when CIT exceeded ~10 hours.
Conclusions: Clinical-grade cryopreserved hepatocytes retain viability and function for over a decade. CIT, donor BMI, and age most affected post-thaw quality, while WIT and storage duration had minimal impact. These findings support refining donor selection to improve cryopreservation outcomes.
The authors would like to thank the Hepatocyte Isolation Team at King’s College Hospital for technical support and the Liver Transplant Unit for providing access to donor tissue and the patients and families who consented to tissue donation for research purposes. This study was supported by a PhD studentship from the Republic of Türkiye Ministry of National Education..
[1] Primary human hepatocytes (PHHs)
[2] hepatocyte transplantation
[3] cryopreservation
[4] donor age
[5] cold ischemia time (CIT)
[6] body mass index (BMI)